Excision Of Meningioma
Thailand
-
Our Price USD 12140
-
Hospital Price USD 12779
-
You Save : USD 639
Booking Amount: USD 1214. Pay Remaining 90% at the hospital.
Book NowAdditional Credit
Among the important extras we offer as part of the Additional Credit are the following:
-
Site Tourism For The Patient & Attendant
-
Airport Pick & Drop Service
-
Ambulance service at airport
-
Priority appointments with The Doctor
-
Cancel Easily Anytime with Full Refund
-
Room Upgradation
-
Free Online Doctor Consultation Valued at USD 20
-
Free hotel Stay for 5 to 7 days Accordingly
-
Welcome Kit at Arrival
-
Interpreter
-
Medical Visa Assistance
What is Included?
- Doctor consultation charges
- Lab tests and diagnostic charges
- Room charges inside hospital during the procedure
- Surgeon Fee
- Cost of implant
- Nursing charges
- Hospital surgery suite charges
- Anesthesia charges
- Routine medicines and routine consumables (bandages, dressings etc.)
- Food and Beverages inside hospital stay for patient and one attendant.
What is not Included?
- Extra Radiology Investigations
- Healthcare Professionals Charges of other consultations.
- Other Requested Services such as Laundry etc.
- Additional Pharmaceutical Products and Medicines After Discharge from Hospital.
- Management of Conditions Unrelated to Procedures or Pre-Existing.
- The cost of any additional implants will be in addition to the package cost.
Package Description
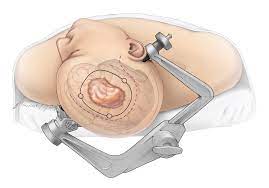
Excision Of Meningioma:
A craniotomy is the most common procedure for removing a meningioma. Making an incision in the scalp and extracting a portion of bone from the skull are both part of this surgery. The neurosurgeon can then access the tumour and remove it, or as much of it as possible, without causing significant brain damage.
Disease Overview:
Brain Tumour
A brain tumour is an abnormal cell growth in the brain's tissues. Brain tumours can be benign (no cancer cells) or malignant (fast-growing cancer cells). Some of them are primary brain tumours, meaning they begin in the brain. Others are metastatic, which means they begin elsewhere in the body and spread to the brain.
As new cells replace old or damaged ones, normal cells proliferate in a regulated manner. Tumor cells multiply uncontrolled for reasons that are unknown.
A primary brain tumour is a benign tumour that begins in the brain and seldom spreads to other regions of the body. Primary brain tumours can be either benign or cancerous.
A benign brain tumour develops slowly, has well-defined borders, and spreads only infrequently. Benign tumours can be life threatening if they are placed in a key region, despite the fact that their cells are not cancerous.
A malignant brain tumour spreads to neighbouring brain regions, develops swiftly, and has irregular borders. Malignant brain tumours, despite their common name, do not meet the criteria of cancer since they do not spread to organs outside of the brain and spine.
Metastatic (secondary) brain tumours start out as cancer in another part of the body and then spread to the brain. When cancer cells are transported through the bloodstream, they develop tumours. Lung and breast cancers are the most prevalent malignancies that spread to the brain.
A brain tumour, whether benign, malignant, or metastatic, can all be life-threatening. The brain can't expand to make place for a growing mass since it's encased in a bony skull. The tumour compresses and displaces normal brain tissue as a result.
Some brain tumours cause the cerebrospinal fluid (CSF) that circulates around and through the brain to become clogged. This obstruction raises intracranial pressure and can cause the ventricles to expand (hydrocephalus). Swelling is a symptom of certain brain tumours (edema). The "mass effect" is caused by the size, pressure, and swelling of the body, which causes many of the symptoms.
Disease Signs and Symptoms:
Tumors can cause damage to the brain by killing healthy tissue, squeezing healthy tissue, or raising intracranial pressure. The kind, size, and location of the tumour in the brain all influence the symptoms. Symptoms in general include:
- Seizures with headaches that seem to get worse in the morning
- stumbling, dizziness, and walking difficulties
- issues with speech (e.g., difficulty finding the right word)
- irregular eye movements, visual difficulties
- Increased intracranial pressure due to weakness on one side of the body produces sleepiness, headaches, nausea and vomiting, and slow reactions.
The following are examples of specific symptoms:
Behavioral and emotional problems; poor judgement, motivation, or inhibition; decreased sense of smell or visual loss; paralysis on one side of the body; lower mental ability and memory loss are all possible adverse effects of frontal lobe tumours.
Parietal lobe tumours can cause difficulty with speaking, writing, drawing, and naming, as well as lack of recognition, spatial impairments, and eye-hand coordination.
Vision loss in one or both eyes, visual field cuts, fuzzy vision, illusions, and hallucinations are all possible symptoms of occipital lobe tumours.
Temporal lobe tumours can cause issues with speaking and interpreting language, as well as short- and long-term memory.
aggressiveness on the rise
Behavioral and emotional problems, trouble speaking and eating, tiredness, hearing loss, muscular weakness on one side of the face (e.g., head tilt, crooked grin), uncoordinated walking, drooping eyelid or double vision, and vomiting are all symptoms of brainstem tumours.
Increased hormone secretion (Cushing's Disease, acromegaly), cessation of menstruation, irregular milk secretion, and diminished libido are all possible side effects of pituitary gland tumours.
Disease Causes:
hereditary illnesses, such as neurofibromatosis, extended exposure to pesticides, industrial solvents, and other toxins cancer elsewhere in the body
Information related to Treatment
Package Details
Days in Hospital
4 Days
Days in Hotel
*
8 Days
Room Type
Private

Treating Doctor
Dr. Paisan Vachatimanont
Neurologist- Behavioral neurology, Neurodevelopmental disabilities, Vascular neurology, Neurotrauma, Endovascular Neurosurgeon, Neurology, Neurological Disorders, Neurovascular Surgery
Bumrungrad International Hospital Bangkhen, Thailand
40 Years of Experience

Treating Doctor
Dr. Methee Wongsirisuwan
Neuro surgeon- Minimal Invasive Neurosurgery, Endoscopic Neurosurgery
Bumrungrad International Hospital Bangkhen, Thailand
31 Years of Experience

Treating Doctor
Dr. Nanthasak Tisavipat
Neuro surgeon- surgical clipping of intracranial aneurysms, Cerebral Palsy Treatment, Cerebral Angiogram, Brain Surgery and Brain Aneursym Surgery, Endovascular coiling, MVD, MST
Bangkok Hospital Bangkok, Thailand
26 Years of Experience

Treating Doctor
Dr. REANCHAI JULAVISETKUL
Neurologist- Neuromuscular medicine, Neurodevelopmental disabilities, Neuroradiology, Neurotrauma, Neurointervention Surgeon, Endovascular Neurosurgeon
Samitivej Hospital Bangkok, Thailand
28 Years of Experience
Treating Doctor
SONGCHAI CHINWATTANAKUL, M.D.
Neurologist- Internal Medicine, Internal Medicine, Internal Medicine, Internal Medicine, Neurology
Samitivej Srinakarin Hospital Bangkok, Thailand
22 Years of Experience

Treating Doctor
Dr. Pornthep Mingmalairak
Neuro surgeon- Brain Specialist, Neurology, Inflammtory diseases of the Nervous System
Sikarin Hospital Bangkok, Thailand
22 Years of Experience

Treating Doctor
Dr. Nanthasak Tisavipat
Neuro surgeon- surgical clipping of intracranial aneurysms, Cerebral Angiogram, Brain Surgery and Brain Aneursym Surgery, Endovascular coiling, MVD, MST, Vagus nerve stimulation (VNS) therapy
Wattanosoth Cancer Hospital Bangkok, Thailand
26 Years of Experience

Treating Doctor
PROF. DR. KONGKIAT KULKANTRAKORN
Neurologist- Brain Tumour Surgery, Pituitary Diseases, Chronic Pain Treatment, Chronic Pain Treatment, CyberKnife Treatment, Neurotomy, MVD, PSR, Arteriovenous malformations (AVMs), Pediatric tumors, Brain Tumour Surgery
Bangkok International Hospital Bangkok, Thailand
28 Years of Experience

Treating Doctor
DR. YOTIN CHINVARUN
Neurologist- Cyber Knife Surgeon, surgical clipping of intracranial aneurysms, Cerebral Angiogram, Brain Surgery and Brain Aneursym Surgery, Endovascular coiling, Neurotomy, MVD, PSR, MST
Bangkok International Hospital Bangkok, Thailand
33 Years of Experience

Treating Doctor
ASST. PROF. DR. PARUNUT ITTHIMATHIN
Neuro surgeon- Brain Tumour Surgery, Cyber Knife Surgeon, Mixed Gliomas, Meningiomas, Brain Tumor, Brain Surgery and Brain Aneursym Surgery, Brain Tumor, Brain Haemorrhage, Minimally invasive neurosurgery, Endoscopic Acoustic Schwanomas, Meningiomas, Arteriovenous malformations (AVMs), Deep Brain Stimulation Surgery, Brain Tumour Surgery
Bangkok International Hospital Bangkok, Thailand
23 Years of Experience