Additional Credit
Among the important extras we offer as part of the Additional Credit are the following:
-
Site Tourism For The Patient & Attendant
-
Airport Pick & Drop Service
-
Ambulance service at airport
-
Priority appointments with The Doctor
-
Cancel Easily Anytime with Full Refund
-
Room Upgradation
-
Free Online Doctor Consultation Valued at USD 20
-
Free hotel Stay for 5 to 7 days Accordingly
-
Welcome Kit at Arrival
-
Interpreter
-
Medical Visa Assistance
What is Included?
- Doctor consultation charges
- Lab tests and diagnostic charges
- Room charges inside hospital during the procedure
- Surgeon Fee
- Cost of implant
- Nursing charges
- Hospital surgery suite charges
- Anesthesia charges
- Routine medicines and routine consumables (bandages, dressings etc.)
- Food and Beverages inside hospital stay for patient and one attendant.
What is not Included?
- Extra Radiology Investigations
- Healthcare Professionals Charges of other consultations.
- Other Requested Services such as Laundry etc.
- Additional Pharmaceutical Products and Medicines After Discharge from Hospital.
- Management of Conditions Unrelated to Procedures or Pre-Existing.
- The cost of any additional implants will be in addition to the package cost.
Package Description
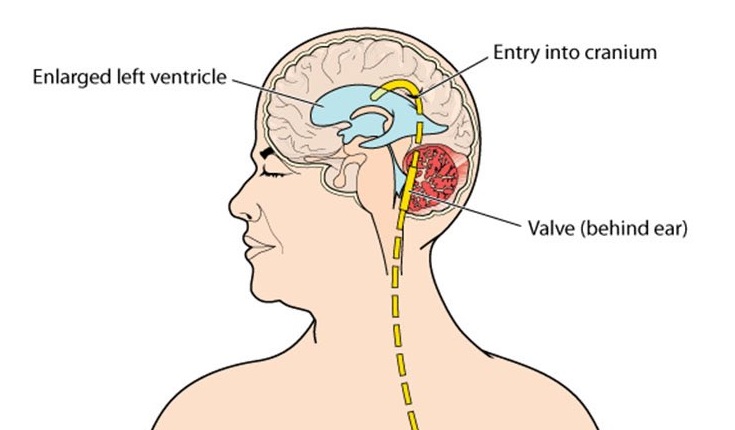
VP Shunt
Ventriculoperitoneal shunting is a procedure that removes excess cerebrospinal fluid (CSF) from the brain's cavities (ventricles) (hydrocephalus). This operation is performed under general anaesthesia in the operating room. To drain excess cerebrospinal fluid, a tube (catheter) is delivered from the cavities of the head to the abdomen (CSF).
Disease Overview:
Hydrocephalus
The collection of fluid in the cavities (ventricles) deep within the brain is known as hydrocephalus. The extra fluid expands the ventricles, which exerts pressure on the brain.
The brain and spinal column are generally bathed in cerebrospinal fluid, which circulates via the ventricles. However, excessive cerebrospinal fluid pressure, which is linked with hydrocephalus, can damage brain tissues and cause a variety of brain function disorders.
Hydrocephalus may strike anybody at any age, however it is more common in newborns and individuals aged 60 and up. Hydrocephalus can be treated surgically to restore and maintain normal cerebrospinal fluid levels in the brain. Managing symptoms or issues caused by hydrocephalus frequently necessitates a variety of treatments.
Disease Signs and Symptoms:
The signs and symptoms of hydrocephalus differ depending on the age at which it first appears.
Infants
In babies, common indications and symptoms of hydrocephalus include:
- Alterations in the brain
- A bulging or tight soft patch (fontanel) on the top of the skull An exceptionally enormous head A fast growth in the size of the head
Symptoms and physical indicators
- Vomiting and nausea
- Sluggishness or sleepiness (lethargy)
- Irritability
- Unhealthy eating habits
- Seizures
- Downward-looking eyes (sunsetting of the eyes)
- Muscle tone and strength problems
Children of all ages, including toddlers and older children
Signs and symptoms in toddlers and older children may include:
Symptoms and physical indicators
- Headache
- Double eyesight or hazy vision
- Eye motions that are abnormal
- Sleepiness or sluggishness Sleepiness or sluggishness in a toddler
- Vomiting or nausea
- Unstable equilibrium
- Coordination issues
- Appetite problems
- Bladder control problems or frequent urination
- Changes in behaviour and cognition
- Irritability
- Personality shifts
- School performance is deteriorating.
- Delays or difficulties with previously learned tasks like walking or talking
Adults in their twenties and thirties
The following are common indications and symptoms in this age group:
- Headache
- Sluggishness
- Coordination or balance problems
- Urinary incontinence or a frequent need to urinate
- Problems with vision
- Memory, focus, and other cognitive abilities decline, which may have an impact on work performance.
Adults in their latter years
The following are the most prevalent indications and symptoms of hydrocephalus in individuals aged 60 and up:
- Urinary incontinence or a frequent need to urinate
- Loss of memory
- Other thinking or reasoning skills are gradually deteriorating.
- Difficulty walking, which is typically characterised as a shuffling stride or a stuck feeling in the feet.
- Coordination or balance issues
Disease Causes:
An imbalance between the amount of cerebrospinal fluid generated and the amount absorbed into the circulation causes hydrocephalus.
Cerebrospinal fluid is generated by the tissues that line the brain's ventricles. It travels through interconnected channels in the ventricles. The fluid ultimately finds its way into regions around the brain and spine. Blood arteries in tissues on the surface of the brain absorb the majority of it.
Cerebrospinal fluid is vital for brain function because it:
- Allowing the comparatively hefty brain to float within the skull by keeping it buoyant.
- To protect the brain from harm, it is cushioned.
- Getting rid of waste materials produced by the brain's metabolism
- Flowing back and forth between the brain cavity and the spinal column to maintain a constant pressure within the brain — compensating for fluctuations in brain blood pressure.
One of the following causes too much cerebrospinal fluid in the ventricles:
Obstruction. A partial obstruction of the flow of cerebrospinal fluid, either from one ventricle to another or from the ventricles to other regions around the brain, is the most prevalent condition.
Absorption is poor. A issue in absorbing cerebrospinal fluid is less prevalent. This is frequently linked to inflammation of brain structures as a result of illness or injury.
Overproduction. Cerebrospinal fluid is occasionally produced faster than it can be absorbed.
Disease Diagnosis:
The following factors are commonly used to make a diagnosis of hydrocephalus:
- Your responses to the doctor's signs and symptoms questions
- A complete physical examination
- An examination of the nervous system
- Tests of the brain
- Examination of the nervous system
The sort of neurological exam a person receives is determined on their age. In the office, the neurologist may ask questions and do basic tests to assess muscle condition, mobility, well-being, and the functioning of the senses.
Imaging of the brain
The following imaging studies can aid in the diagnosis of hydrocephalus and the identification of the underlying causes of the symptoms:
Ultrasound. Because it is a reasonably easy and low-risk technique, this test is frequently used for an initial screening of neonates. The ultrasound equipment is positioned over a soft region on the top of a baby's head called the fontanel.
During standard prenatal checkups, ultrasound may diagnose hydrocephalus before delivery.
MRI. This technique creates comprehensive pictures of the brain using radio waves and a magnetic field. Although this test is harmless, it is loud and demands that you lie motionless.
Excess cerebrospinal fluid can create enlarged ventricles, which can be seen on MRI images. They can also be utilised to figure out what's causing the hydrocephalus or what's causing the symptoms.
Some MRI scans may need minor anaesthesia in children. Some facilities, on the other hand, employ a quick variant of MRI that doesn't require sedation.
CT scan is a type of x-ray. Cross-sectional pictures of the brain are obtained using this specialist X-ray technique. Scanning is rapid and painless. However, because this test necessitates laying motionless, a youngster is frequently given a light sedative.
CT scanning gives less detailed pictures than MRI and involves a tiny level of radiation exposure. CT scans for hydrocephalus are typically reserved for urgent situations.
Disease Treatment:
Hydrocephalus can be treated with one of two surgical procedures.
Shunt
The surgical implantation of a drainage system, known as a shunt, is the most frequent therapy for hydrocephalus. It's made up of a long, flexible tube with a valve that maintains brain fluid flowing in the appropriate direction and at the right pace.
The tube is normally inserted into one of the brain's ventricles on one end. The tube is then tunnelled through the skin to a different portion of the body, such as the belly or a heart chamber, where the extra fluid may be absorbed more easily.
Hydrocephalus patients typically require a shunt system for the remainder of their lives. They must be monitored on a regular basis.
Third ventriculostomy (endoscopic)
For certain patients, endoscopic third ventriculostomy is a surgical technique that can be used. The surgeon examines the interior of the brain using a tiny video camera. To let cerebrospinal fluid to drain out of the brain, your surgeon cuts a hole in the bottom of one of the ventricles or between the ventricles.
Surgical complications
Both surgical treatments have the potential to cause problems. Because of mechanical issues, blockages, or infections, shunt systems can stop draining cerebrospinal fluid or regulate drainage poorly. Ventriculostomy complications include bleeding and infections.
Any failure needs immediate treatment, surgical modifications, or other measures. A fever or return of the previous hydrocephalus symptoms should necessitate a visit to your doctor.
Information related to Treatment
Package Details
Days in Hospital
4 Days
Days in Hotel
*
17 Days
Room Type
Private

Treating Doctor
Dr. Paisan Vachatimanont
Neurologist- Behavioral neurology, Neurodevelopmental disabilities, Vascular neurology, Neurotrauma, Endovascular Neurosurgeon, Neurology, Neurological Disorders, Neurovascular Surgery
Bumrungrad International Hospital Bangkhen, Thailand
40 Years of Experience

Treating Doctor
Dr. Methee Wongsirisuwan
Neuro surgeon- Minimal Invasive Neurosurgery, Endoscopic Neurosurgery
Bumrungrad International Hospital Bangkhen, Thailand
31 Years of Experience

Treating Doctor
Dr. Nanthasak Tisavipat
Neuro surgeon- surgical clipping of intracranial aneurysms, Cerebral Palsy Treatment, Cerebral Angiogram, Brain Surgery and Brain Aneursym Surgery, Endovascular coiling, MVD, MST
Bangkok Hospital Bangkok, Thailand
26 Years of Experience

Treating Doctor
Dr. REANCHAI JULAVISETKUL
Neurologist- Neuromuscular medicine, Neurodevelopmental disabilities, Neuroradiology, Neurotrauma, Neurointervention Surgeon, Endovascular Neurosurgeon
Samitivej Hospital Bangkok, Thailand
28 Years of Experience
Treating Doctor
SONGCHAI CHINWATTANAKUL, M.D.
Neurologist- Internal Medicine, Internal Medicine, Internal Medicine, Internal Medicine, Neurology
Samitivej Srinakarin Hospital Bangkok, Thailand
22 Years of Experience

Treating Doctor
Dr. Pornthep Mingmalairak
Neuro surgeon- Brain Specialist, Neurology, Inflammtory diseases of the Nervous System
Sikarin Hospital Bangkok, Thailand
22 Years of Experience

Treating Doctor
Dr. Nanthasak Tisavipat
Neuro surgeon- surgical clipping of intracranial aneurysms, Cerebral Angiogram, Brain Surgery and Brain Aneursym Surgery, Endovascular coiling, MVD, MST, Vagus nerve stimulation (VNS) therapy
Wattanosoth Cancer Hospital Bangkok, Thailand
26 Years of Experience

Treating Doctor
PROF. DR. KONGKIAT KULKANTRAKORN
Neurologist- Brain Tumour Surgery, Pituitary Diseases, Chronic Pain Treatment, Chronic Pain Treatment, CyberKnife Treatment, Neurotomy, MVD, PSR, Arteriovenous malformations (AVMs), Pediatric tumors, Brain Tumour Surgery
Bangkok International Hospital Bangkok, Thailand
28 Years of Experience

Treating Doctor
DR. YOTIN CHINVARUN
Neurologist- Cyber Knife Surgeon, surgical clipping of intracranial aneurysms, Cerebral Angiogram, Brain Surgery and Brain Aneursym Surgery, Endovascular coiling, Neurotomy, MVD, PSR, MST
Bangkok International Hospital Bangkok, Thailand
33 Years of Experience

Treating Doctor
ASST. PROF. DR. PARUNUT ITTHIMATHIN
Neuro surgeon- Brain Tumour Surgery, Cyber Knife Surgeon, Mixed Gliomas, Meningiomas, Brain Tumor, Brain Surgery and Brain Aneursym Surgery, Brain Tumor, Brain Haemorrhage, Minimally invasive neurosurgery, Endoscopic Acoustic Schwanomas, Meningiomas, Arteriovenous malformations (AVMs), Deep Brain Stimulation Surgery, Brain Tumour Surgery
Bangkok International Hospital Bangkok, Thailand
23 Years of Experience
Similar Packages
Frequently Asked Questions
In Thailand, the typical price of a VP Shunt begins at USD 12500. In Thailand, there are numerous hospitals with JCI and Healthcare Accreditation Institute certifications that provide VP Shunt.
International patients can get VP Shunt from a number of hospitals around the nation. The following are a few of Thailand's top hospitals for VP Shunt: Phyathai 2 International Hospital Bangpakok 9 International Hospital (BPK 9) Bangkok Dusit Medical Services Vejthani Hospital
In addition to the VP Shunt cost, the patient has several further expenses to cover. In this instance, the daily fee might begin at USD $50 per person.
The patient's recovery may differ based on a number of variables. Nonetheless, following release, patients are expected to remain in the nation for roughly 21 days on average. It is advised that patients stay for this length of time in order to finish all required follow-ups and control tests and make sure the surgery went well.
After VP Shunt, the patient is expected to stay in the hospital for around 4 days in order to get treatment and monitoring. The patient is closely watched during the healing process, and control tests are run to make sure everything is in working order. Physiotherapy sessions are often scheduled during hospital recovery, if necessary.
In Thailand, some of the most sought-after physicians for VP Shunts include: Dr. Chakri Thanyonpaporn Dr. Nantawat Lerdkittipat Dr. Sombat Muengtaweepongsa Dr. Yongsakdi Liengudom Dr. Wasuwat Sookkee
In Thailand, there are around four hospitals that provide VP Shunt. These hospitals have the necessary facilities, including a special treatment facility. Furthermore, it is well known that these institutions treat patients in accordance with both local and international legal needs and standards.