Microdiscectomy Surgery cost in India
The cost of Microdiscectomy Surgery in India ranges from USD 3800 to USD 10000
Procedure Description
Microdiscectomy Surgery
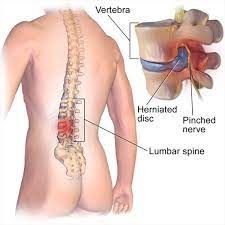
Large wounds, protracted recuperation times, and agonizing rehabilitation were standard after spinal surgery. Thankfully, improvements in surgery, such as the microdiscectomy operation, have made the process better. Patients with a herniated lumbar disc can have a less invasive surgical treatment termed a microdiscectomy, which is also occasionally referred to as a micro-decompression or microdiskectomy.
In order to relieve pressure on the spinal nerve column, a surgeon will remove some of the herniated disc during this procedure.
Disease Overview
The cushions between the vertebrae in the upper back and neck are known as cervical discs. The nucleus pulposus, the gelatinous inner disc material, ruptures or herniates through the outer cervical disc wall, causing herniation. When the protective outer layer of a disc splits, some of the nucleus pulposus seeps into the tear, the result is a herniated disc. When the nucleus pulposus, which contains inflammatory proteins, spills out of the disc and onto a neighbouring nerve root, it produces the most agony. A herniated disc is less likely to spill onto the spinal cord.
Disease Sign an Symptoms
The following are some of the most typical indications and symptoms of a herniated cervical disc:
Neck ache. The discomfort usually radiates from the back or side of the neck. It might be anything from a little ache that is painful when touched to a searing or scorching agony.
Pain in the radicles. A pinched nerve in the neck can cause discomfort to spread down the shoulder, arm, hand, and/or fingers. It might feel hot or electric shock-like at times.
Cervical radiculopathy is a condition that affects the nerves in the neck. Numbness and/or weakness in the shoulder, arm, hand, and/or fingers can also be caused by a pinched nerve or nerve root inflammation. In rare cases, radiculopathy is accompanied with radicular discomfort.
Specific head postures or activities exacerbate symptoms. The pain from a herniated disc tends to flare up and get worse when you do things like play sports or lift a big weight. It's also possible that certain head postures, such as twisting to one side or tipping the head forward, aggravate the discomfort.
Stiffness in the neck A cervical herniated disc's pain and inflammation might limit some neck motions and impair range of motion.
Disease Causes
The following are some of the most common reasons of a herniated disc in the neck:
-Degeneration of the discs over time. A disc loses moisture as it ages, making it less flexible and durable. A disc with a decreased water content is more likely to develop cracks and rips.
-Trauma. A disc can rupture or herniate as a result of a direct trauma on the spine.
-Herniated discs can also be caused by connective tissue problems or other anomalies in the spine, which are less prevalent causes.
Risk Factor:
The likelihood of suffering a herniated disc rises with age. A cervical herniated disc is most likely to occur between the ages of 30 and 50, according to some estimations. Men have been reported to be at higher risk for a cervical herniated disc in most studies, but a new study reveals that women may also be at higher risk. In the adult population, the rate of cervical herniated discs is believed to be between 0.5 percent and 2 percent. Many cases of cervical herniated disc go undetected, and estimates may differ by population.
Disease Diagnosis
A cervical herniated disc is normally diagnosed using a three-step process:
Patient's medical history. The patient's medical history is examined, including any chronic illnesses, previous injuries, or back or neck problems. Also obtained is information about the present symptoms.
Examination of the body. Any regions of swelling, soreness, or discomfort in the neck can be palpated (felt). The doctor then examines the range of motion in the neck, as well as any evidence of neurological abnormalities in the arms, such as numbness, weakness, or trouble with reflexes.
Imaging research. An imaging study can reveal whether a disc has begun to flatten or shift out of its natural position. Because of the high-quality image of soft tissues provided by an MRI scan, it is the recommended approach for examining a herniated disc. A CT or CT myelogram may be used instead of an MRI if an MRI is not available.
In many circumstances, the patient history and physical examination provide enough information to begin therapy, therefore an imaging investigation is not necessarily sought immediately once. To identify a cervical herniated disc as the source of discomfort, a patient's history, physical exam, imaging study, and an x-ray guided, contrast-enhanced diagnostic injection are usually compared.
Disease Treatment
When a cervical herniated disc first forms or flares up intermittently, such as during exercise, it is usually the most painful. A brief time of rest and/or activity reduction is recommended if the neck discomfort is severe and/or radiates down the arm or hand. Here are a few examples:
Refraining from rigorous activities such as physical work or sports participation
Avoiding motions that aggravate discomfort, such as moving one's head to one side.
Moving your sleeping posture, such as changing your pillow and/or sleeping on your back rather than your side or stomach
Medications
Nonsteroidal anti-inflammatory medicines (NSAIDs) are medications that assist the body decrease inflammation. Because nerve root and other tissue inflammation contributes to some of the severe pain induced by a herniated disc,
Surgery for a Herniated Disc in the Cervical Spine
The following are some of the most prevalent forms of surgery for a herniated disc in the neck:
Spine fusion with anterior cervical discectomy (ACDF)
ACDF surgery is the most frequent procedure used by spine surgeons to repair a herniated disc in the neck. The disc is extracted through a one-inch incision in the front of the neck during this procedure. After the disc is removed, the disc area is prepared for the neighbouring vertebrae to grow together and fuse. For extra stability and maybe a higher fusion success rate, a plate can be placed in front of the graft.
Artificial disc replacement in the cervical spine
Artificial disc replacement surgery, like ACDF surgery, involves removing the damaged disc through a tiny incision at the front of the neck. An artificial disc is placed in the disc space between the neighbouring vertebrae instead of fusing the surrounding vertebrae. The artificial disc's purpose is to replicate the original disc's shape and function.
Cervical discectomy in the back
This procedure is comparable to a lumbar discectomy performed from the back. For cervical discs that herniate laterally into the neural foramen, it may be a viable option (the tunnel that the nerve travels through to exit the spinal canal).
Because there are many veins in this location that might induce bleeding, and bleeding reduces visibility during surgery, this posterior approach is more challenging than an anterior approach. This method also demands greater spinal manipulation, which increases the risk of complications.
Country wise cost comparison for Microdiscectomy Surgery:
| Country | Cost |
|---|---|
| India | $4320 |
| Turkey | $6746 |
Treatment and Cost
14
Total Days
In Country
- 1 Day in Hospital
- 2 No. Travelers
- 13 Days Outside Hospital
Treatment cost starts from
$4800
Popular Hospital & Clinic
Featured Hospital
0 Hospitals
Related Packages
More Related Information
Some of the top rated hospitals are:
- Saudi Arabia